Abstract
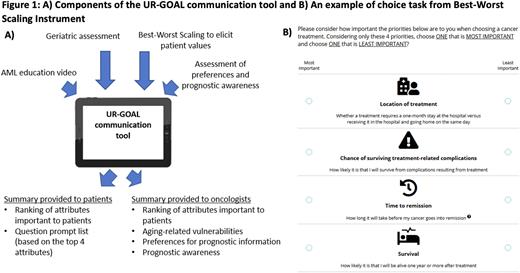
Introduction: Aging-related vulnerabilities (e.g. functional impairment) are prevalent in older adults with AML and can affect the risks and benefits of treatment. Shared decision making (SDM) is an important component of patient-centered care. To achieve SDM, patients must be informed about their disease, treatment options, and prognosis, and their values should be incorporated into treatment decisions. We previously developed and adapted a patient-centered communication tool [University of Rochester-Geriatric Oncology Assessment for acute myeloid Leukemia (UR-GOAL)] for older adults with AML (Figure 1a). The UR-GOAL tool assesses aging-related vulnerabilities, patient values, and prognostic awareness among older patients with AML. In this study, we assessed the feasibility and usability of the UR-GOAL tool for use in AML treatment decision making.
Methods: We conducted a single arm pilot study at the Wilmot Cancer Institute and affiliated community oncology practices. We recruited adults (≥60 years) with newly diagnosed AML, their caregivers, and oncologists. The UR-GOAL tool includes: a) AML educational video, b) geriatric assessment to assess aging-related vulnerabilities, c) Best-Worst Scaling to assess patient values (Figure 1b), and d) assessment of prognostic awareness. A summary report is provided to the patient and oncologist at completion of the tool. The primary feasibility metric was retention rate (>50% was considered feasible). We collected recruitment rate, usefulness (Preparation for Decision Making Scale, range 1-5; higher is better), usability, and clinical outcomes including AML knowledge (range 0-14, higher is better), perceived efficacy in communicating with the oncologist (range 5-25, higher is better), SDM (SDM-Q-9, range 0-100; higher is better), and patient-centered communication (PCC-Ca, range 0-5; higher is better). We used paired t-tests or Wilcoxon signed-rank tests to assess changes in measures from baseline to post-intervention. Due to the pilot nature of the study and small sample size, hypothesis testing was performed at α=0.10 (2-tailed). We conducted post-intervention qualitative interviews to gather feedback.
Results: We included 15 patients (mean age=76, range 64-88), 12 caregivers (mean age=69 years, range 47-86), and 5 oncologists. Most patients (93%) were white and non-Hispanic. Enrollment rate was 84% and retention rate was 73%. Mean scores on the Preparation for Decision Making Scale were 3.8 (SD 0.7) and 3.5 (SD 1.2), among patients and caregivers, respectively. On usability survey, majority of patients (>90%) agreed that the UR-GOAL tool helped them understand AML and its treatment options, identify questions for their doctor, understand their values, and make more informed decisions.
At baseline, mean AML knowledge scores among patients and caregivers were 6.0 (SD 1.1) and 5.7 (SD 1.3), respectively, which increased to 6.6 (SD 1.7; p=0.22) and 7.3 (SD 0.8; p=0.03) post-intervention. Perceived efficacy in communicating with the oncologist increased from baseline to post-intervention for both patients [mean +1.5 (SD 3.0; p=0.15)] and caregivers [mean +1.6 (SD 1.6; p=0.02)]. At post-intervention, mean patient scores on SDM-Q-9 and PCC-Ca were 89.4 (SD 14.4) and 4.4 (SD 0.5), respectively. Mean score on PCC-Ca was 93.5 (SD 8.1) for caregivers. Together, these scores indicate high level of SDM and patient-centered communication.
In qualitative interviews, patients felt the educational video was easy to understand and suggested that they have the opportunity to re-watch the video as needed. Patients found the summary report helpful, and one patient noted referencing the report during subsequent visits with their oncologist. Oncologists did not perceive the tool to be burdensome to them or patients, and felt the summary report was easy to interpret. Oncologists felt the tool provided them with useful insight into the patient's understanding of their diagnosis and prognosis.
Conclusion: We demonstrated it is feasible to incorporate a patient-centered communication tool to support older patients with AML, their caregivers, and oncologists in making treatment decisions. The UR-GOAL tool may improve patient and caregiver knowledge of AML and perceived efficacy in interacting with the oncologist. A pilot randomized controlled trial is ongoing to evaluate the preliminary efficacy of the UR-GOAL tool on SDM and communication.
Disclosures
Liesveld:Blueprint Sciences: Membership on an entity's Board of Directors or advisory committees; BMS: Membership on an entity's Board of Directors or advisory committees; Servier: Membership on an entity's Board of Directors or advisory committees; Pharmacosmos: Membership on an entity's Board of Directors or advisory committees; SYROS: Other: DSMB. O'Dwyer:BEAM Therapeutics: Consultancy. Loh:Seattle Genetics: Consultancy; Pzifer: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal